Hi guys,
Forgot to let you know but I've moved. So if you still want to read my blurp then head over to my WordPress page.
Tuesday 6 November 2018
Friday 15 June 2018
Metal Nurse: Acquired Brain Injury
I had already previously written about mental health, here and here. Recently due to unforeseen circumstances, I saw myself return to that field on a full-time basis. I still keep one hand in the acute sector because the experience you get there is second to none. Now the job I've moved into involves taking care of patients with Acquired Brain Injury(ABI), sometimes known as Traumatic Brain Injury. An area I didn't really think I'd have any interest in. But here I am. Since starting what has become a little evident is that ABI is often the condition that no ones know how to manage properly or wants to deal with. Sometimes it is pushed into the learning disabilities section, other times it put under the mental health umbrella or even put under the general health. What really has come to light is it is a syndrome that is so multi-faceted it needs input from all specialities, because it affects so many aspects of people's health. But whilst the patient who has the condition should be the focus, there has to be some work done with the family and friends of the patient. Because the person who they used to love and care for has changed, sometimes temporarily but more often than not permanently. It is a major global concern, but somehow often gets missed during a discussion regarding healthcare organisations and re-organisations. This is mostly because treating patients with ABI is expensive, it costs the NHS around £15 billion per year. In the US this is number is $60.43 billion.
So what exactly is ABI?
Well... Broadly speaking it is damage to the brain that happens after you are born. Whether it's due to a traumatic event such as an accident, assault or any other cause such as head injury and/or neurosurgery. Or could be damaged due to diseases, such as meningitis or encephalitis, poisoning, stroke, tumours, substance abuse and so on and so forth. It does not cover brain injury that occurs due to degenerative diseases such as Wilsons Disease or Neuroferritonopathy, or dementia. Some professionals do prefer to use the term Acquired Brain Injury as an umbrella term opposed to Traumatic Brain Injury. The reason being that Traumatic Brain Injury would cover head injuries caused by external forces such as those mentioned above as opposed to internal ones like meningitis etc. Possibly the most famous ABI patient has to be a gentleman named Phineas Gage. There is an excellent Wikipedia page about him, but for those who do not feel like they have enough time to read it, I'll try to summarise what happened. Mr Gage was a railroad worker who was survived an accident where a metal rod went through his skull, it went up through the left side of his skull just above his mandible as he was about to speak, behind his left eye and out at the top of his skull. Destroying large parts of his left frontal lobe in the process. Somehow he survived this and managed to live a relatively full life after the fact. But according to his friends and family, his personality completely changed. It took a few years but he did manage to regain a lot of his social skills and personal skills, but we are still not quite sure as to how. His case has been used to both prove and disprove a lot of hypothesis and theories regarding neurology, the physiology of the brain, and recovery models for patients with ABI
It is a very common injury, in the US, for example, it is estimated that over 5 million people are living with disability due to their brain injury. In the UK it appears to be a bit harder to find numbers on how many people are living with ABI, the numbers wary anywhere between 60.000 and 900.000, though Centre for Mental Health puts the number somewhere around 1.3 million people, with the highest number of affected being aged 15-24 years of age. But the latest statistics according to the head injury charity Headway makes a sobering reading nonetheless. In 2013-2014 there were a total of 348.934 admissions into hospitals due to ABI. If you break down those numbers a little further, head injury admission account for 162.544, of those 100.831 is men. Interestingly researchers in the Department of Neurosurgery, Tianjin Neurological Institute in China did a systematic review regarding worldwide statistics of causes of ABI/TBI. What they found was that in Europe the largest cause of ABI was work-related or caused by falls, in Asia it was largely due to Motor Vehicle Collisions and the in the US mostly sports related. Basically what happens is that men take bigger risks, this could all be part of a larger part of the discussion regarding toxic masculinity. Due to this disproportionate occurrence is why there are not as many services for female patients with ABI. The report by Centre for Mental Health states that a person who suffers from ABI is at double the risk of developing a mental health problem, regardless of whether they had no past history of mental illness. What it also showed was that around 60% of criminal offenders had some sort of brain injury, most of the time this turns out to be an accumulative injury. This is also a common occurrence with those who play contact sports on a regular basis, such as rugby, American Football, and football (Soccer to you barbarians). This also highlights the importance of safety equipment such as helmets and padding.
What are the effects of ABI?
The effect of ABI is varied. It affects every aspect of the persons being, whether emotional, psychological or physical. The most obvious and possibly most common one is the loss of inhibition, loss of emotional control and issues with the memory. The aspect that possibly puts the biggest strain on patients with ABI and their closest, is the loss of insight, loss of empathy and loss of sympathy. Patients with ABI can come across like they have dementia, though what has been found out is that patients who have ABI are more likely to develop dementia later in life. The symptoms of ABI largely depends on what part of the brain has been injured. The most common area to be injured are the frontal lobes, this area is vital for forming memories, empathy, expressive language and more. With damage to the frontal lobe, changes to the personalities are more evident than when other areas of the brain are damaged. Hence the bigger social cost of ABI and managed, alongside the patient's rehabilitation. It can be distressing for both the patient and their loved ones when they lose the ability to put themselves in someone else's situation or say/do things that could be considered outside of the social norms. And they then cannot understand why other people are either upset with them or cannot relate to them. They cannot reflect on their behaviour, or do not see a problem with their behaviour and its impact on others. Disinhibition is a prevalent change that happens to ABI patients, alongside impulsiveness. They become more irritable, they get angrier quicker, with less patience for others and any interruptions to their concentrations. This often results in those patients becoming violent towards their carers and relatives. Aphasia is, according to the National Aphasia Association,
There is also Ataxia, which according to the Ataxia UK,
The most common physical health complaint that occurs to patients post head injury is epilepsy. Epilepsy is a category of neurological disorders that are defined by epileptic seizures. These seizures can come in many forms such as:
These seizures can be short and only happen once, or they can be long and come upon in groups. Typically these are brought upon due to external triggers, such as flickering lights, environmental noises, poor diet (for example badly managed diabetes or excessive amount of stimulants like caffeine and sugar) etc. But with patients who have ABI, they more often occur due to internal triggers such as lack of sleep, stress, emotional excitement and boredom. Those who have ABI tend to be put on anti-epileptic medication prophylactically in order to prevent them from having seizures. Most seizures tend to be self-terminating but carers and family need to have rescue medicines such as buccolam, which is an oral solution, or rectal diazepam in order to cut those seizures short, especially if the patient has had more than the one seizure. Then there is Status Epilepticus, this is a seizure that lasts for longer than five minutes. It is an emergency situation often requiring intensive care input. The prognosis for patients who suffer from status epilepticus is not good, between 10%-30% of those who are diagnosed with it die within a month. Hence the need for speedy treatment, with optimisation of their medications and daily routines, such as strict sleeping regimes.
As can be read this is a very big topic to write about, and there are issues that I have not touched upon. As I have mentioned frequently, this is a major global health concern. It has a multi-faceted impact. It does not just impact on the patient who suffers from the injury, it also affects their friends and family. But not just that due to the disability that comes with it and given the age it occurs most commonly, it can also affect the larger economy. The rehabilitation can take months if not years if they were in employment they will either have to take a long period off in order to return or never return at all. There is a definite need for more centres that provide rehabilitation and treatment for ABI, and this can only be beneficial to everyone. Not just those directly affected.
For further information, I wholeheartedly recommend an organization called Headway who dedicate themselves solely to those who are affected by head injuries.
So what exactly is ABI?
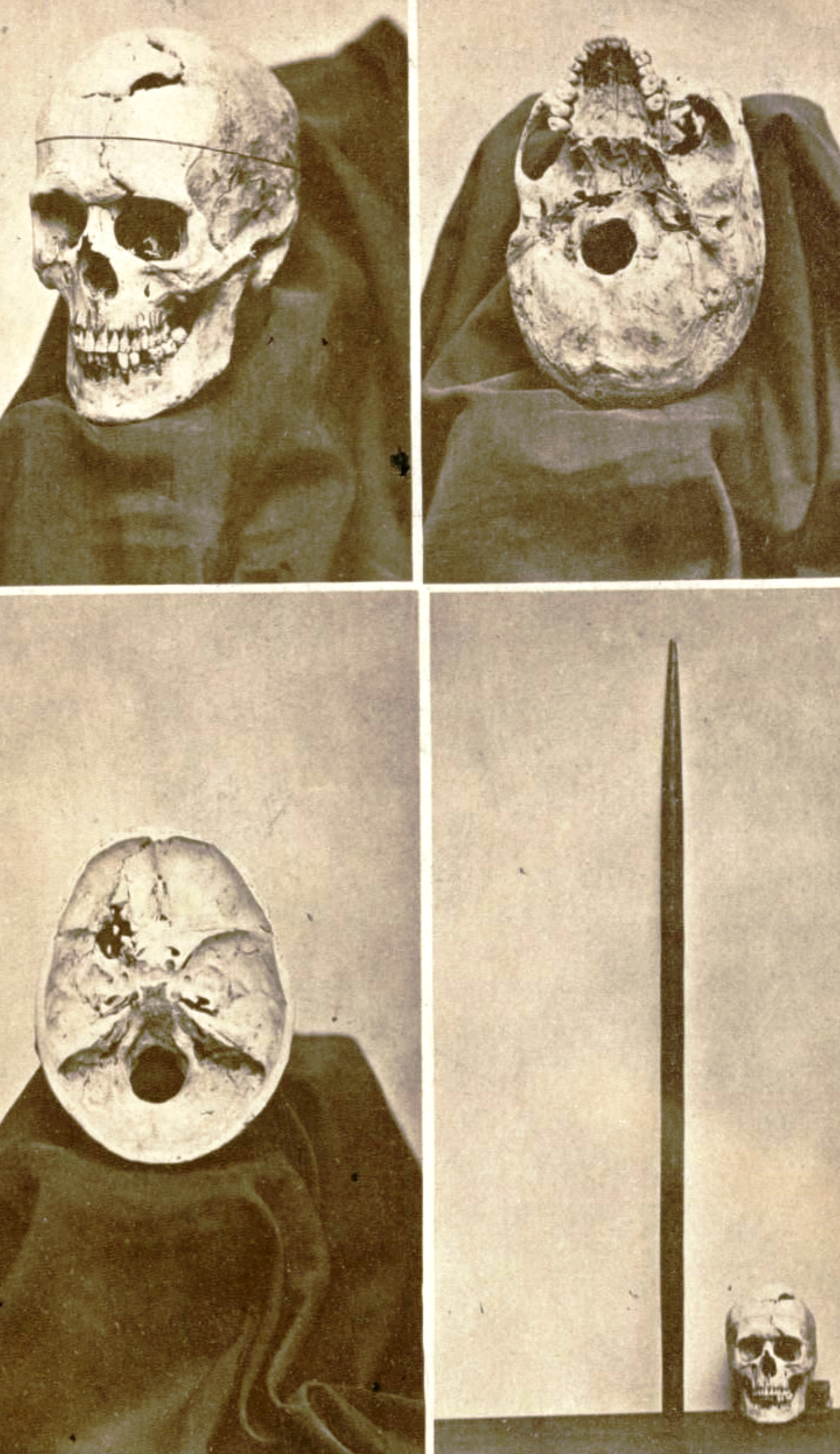 |
| Gage's skull and the iron rod |
 |
| Helmets prevent ABI |
What are the effects of ABI?
 |
| Brain MRI. |
"Aphasia is an impairment of language, affecting the production or comprehension of speech and the ability to read or write."This inability to be able to say what you mean to say, or form the right words, or sentences, can become very frustrating for the patient. And their closest. It can have a major impact on their rehabilitation and recovery.
There is also Ataxia, which according to the Ataxia UK,
"Ataxia’ is an umbrella term for a group of neurological disorders that affect balance, coordination and speech. There are many different types of ataxia that affect people in different ways. "One of the more challenging aspects of these patients care in my view is something called "Cognitive Fatigue". This is where a patient gets more tired and has greater difficulty in concentrating on things that they used to be able to do with ease prior to their injury. This can lead to fluctuation in their mood and difficulties with their emotions and behaviour. Thankfully with the right support, and right support network this can be overcome through intensive rehabilitation.
The most common physical health complaint that occurs to patients post head injury is epilepsy. Epilepsy is a category of neurological disorders that are defined by epileptic seizures. These seizures can come in many forms such as:
- tonic-clonic seizures, also known as grand mal.
- focal seizures
- Absences seizures
- Atonic seizures, also known as drop attacks
These seizures can be short and only happen once, or they can be long and come upon in groups. Typically these are brought upon due to external triggers, such as flickering lights, environmental noises, poor diet (for example badly managed diabetes or excessive amount of stimulants like caffeine and sugar) etc. But with patients who have ABI, they more often occur due to internal triggers such as lack of sleep, stress, emotional excitement and boredom. Those who have ABI tend to be put on anti-epileptic medication prophylactically in order to prevent them from having seizures. Most seizures tend to be self-terminating but carers and family need to have rescue medicines such as buccolam, which is an oral solution, or rectal diazepam in order to cut those seizures short, especially if the patient has had more than the one seizure. Then there is Status Epilepticus, this is a seizure that lasts for longer than five minutes. It is an emergency situation often requiring intensive care input. The prognosis for patients who suffer from status epilepticus is not good, between 10%-30% of those who are diagnosed with it die within a month. Hence the need for speedy treatment, with optimisation of their medications and daily routines, such as strict sleeping regimes.
As can be read this is a very big topic to write about, and there are issues that I have not touched upon. As I have mentioned frequently, this is a major global health concern. It has a multi-faceted impact. It does not just impact on the patient who suffers from the injury, it also affects their friends and family. But not just that due to the disability that comes with it and given the age it occurs most commonly, it can also affect the larger economy. The rehabilitation can take months if not years if they were in employment they will either have to take a long period off in order to return or never return at all. There is a definite need for more centres that provide rehabilitation and treatment for ABI, and this can only be beneficial to everyone. Not just those directly affected.
For further information, I wholeheartedly recommend an organization called Headway who dedicate themselves solely to those who are affected by head injuries.
Tuesday 24 April 2018
Metal Nurse: Open visiting hours
This is possibly going to be the most controversial article I have written. At least amongst my nursing colleagues. It is regarding the dreaded creature called "Visitors". A lot of hospitals in the UK have rather strict visiting hours, often 1400-1600 and 1800-2000, sometimes less, sometimes more. Children wards would often have more lax hours because parents want to be with their kids and the kids want their parents. Not entirely sure where this practice came from or why. There are a lot of reasons bandied about, like that it is protected mealtime hours. Or it is to reduce the infection rate. But honestly, I suspect it is because most nurses just want to get on with their work without being questioned too much. But as a profession, we tend to forget that these relatives are people, people with worries for their loved ones.
Recently a relatively local hospital to me announced that they will change and extend the visiting hours. At first, my initial instinct was "NOOOOOOOOOO". But then when I started thinking about it I warmed up to the idea. Those strict visiting hours are a probably more of a nuisance because what happens is that visitors throng outside the unit, quite a few of them will try and be cheeky and ask if they can be let in earlier. A fair few of those get angry and start raising their voice, especially at the secretaries who like everyone else are just trying to do their job and do not deserve to be shouted at by people who most likely don't know how hospitals work. Then when the visitors do come in, they come in a drove. Then they form a line in asking a multitude of questions, usually when you are a little busy. They are concerned and worried and want to know what is happening to their loved ones and there is nothing really wrong with that. But when you are busy trying to help someone else it becomes frustrating, and because of confidentiality, you can't divulge why you are busy. So the visitors start to think you are rude and you as a nurse start to think that the visitors are self-centred, both of those assumptions are wrong. But it does get in the way of nurses and doctors work when they are halted in their duty, they do want to make sure that the patients are well cared for and do want to answer any queries and alleviate any worries that are voiced. One of the many problems we face as nurses as that as a profession we are very regimented and task-oriented, which can stifle good care and is not very conducive for the patients. I can hear my colleagues spit and spittle and go "Well, I'm not." I'm afraid that most of you are. This does include me, I know full well that I am and I do try my best to not be. We need to be better.
Now. This is not going to be a popular opinion. But... I think that the above-mentioned hospital is correct in extending the visiting hours. Visitors do have their own lives to lead, their own needs that need to be met. So why do they have to organize their lives around those visiting hours? With those new hours, the visitors can come in dribs and drabs as opposed to coming in like a slow mowing gnu herd which makes everyone miserable. A patient with a large family can have one or two people visiting them throughout the day as opposed to having a whole tribe sat around the bed space, potentially annoying the rest of the patients and their visitors in that bay. Not to mention the issues with parking, which does seem to peak at visiting hours.
A lot of hospitals started giving relatives and friends of patients with relatives access to the ward outside normal visiting hours, after a campaign called 'John's Campaign' which has been extremely helpful to both patients and the professionals that take care of them. The thing is that more liberal visiting hours is better for patient care. You get fewer complaints, the patients get better quicker and they tend to be more settled during their stay. Patients satisfaction of their care improves. Which is always excellent. If visitors come in more infrequently this also gives nurses time to educate both the patient and their visitors, especially in terms of self-management and health promotion, which ideally should be part of all good care. Or it gives you enough time to figure out what happened, why it happened and how (hopefully) it can be prevented from happening again. Because collateral history can make such a big difference in patients care.
It is by no means perfect, but to be honest it doesn't have to be. We are there to try and make sure that the patient gets better. And opening the visiting hours does exactly that.
 |
| Usual reaction |
Now. This is not going to be a popular opinion. But... I think that the above-mentioned hospital is correct in extending the visiting hours. Visitors do have their own lives to lead, their own needs that need to be met. So why do they have to organize their lives around those visiting hours? With those new hours, the visitors can come in dribs and drabs as opposed to coming in like a slow mowing gnu herd which makes everyone miserable. A patient with a large family can have one or two people visiting them throughout the day as opposed to having a whole tribe sat around the bed space, potentially annoying the rest of the patients and their visitors in that bay. Not to mention the issues with parking, which does seem to peak at visiting hours.
A lot of hospitals started giving relatives and friends of patients with relatives access to the ward outside normal visiting hours, after a campaign called 'John's Campaign' which has been extremely helpful to both patients and the professionals that take care of them. The thing is that more liberal visiting hours is better for patient care. You get fewer complaints, the patients get better quicker and they tend to be more settled during their stay. Patients satisfaction of their care improves. Which is always excellent. If visitors come in more infrequently this also gives nurses time to educate both the patient and their visitors, especially in terms of self-management and health promotion, which ideally should be part of all good care. Or it gives you enough time to figure out what happened, why it happened and how (hopefully) it can be prevented from happening again. Because collateral history can make such a big difference in patients care.
It is by no means perfect, but to be honest it doesn't have to be. We are there to try and make sure that the patient gets better. And opening the visiting hours does exactly that.
Sunday 15 April 2018
Metal Nurse: Cancer quackery and the vultures that peddle them
There are few things that gets my blood boiling like cancer quackery. I am not going to pretend that I am as knowledgeable as the revered oncology surgeon Orac over at Respectful Insolence. But during both my professional time as a nurse and studying as a student nurse I have come across my fair share of despicable behaviour from people who proclaim themselves as some sort health care professionals, especially when it comes to cancer. Cancer is serious business, it is not something to take lightly. I abhor these vultures who flock around those who have been diagnosed with cancer, and worse still when they flock around the family and whisper such nonsense like "Gerson Therapy works better", "They are too acidotic, bicarb will cure them" and so on and so forth. They convince patients that evidence-based medicine cannot help but that faith-based healings, such as herbal medicine and homoeopathy, will. Then when the patient dies from their cancer they wash their hands of them and say that "Science does not know everything". Leaving a trail of destruction and sorrow in their path, whilst sowing seeds of doubt regarding real medical professionals who then have to pick up the pieces.
These vultures need to be stopped.
One of the main points to keep in mind regarding cancer is that there are at least 100 different types of cancers known. Each with their own pathophysiology's, each with their own characteristics and each with different ways of treatment. So when you see someone that claims that they can cure cancer or know how. Ask them which type of cancer, then ask them how.
Thankfully, Cancer Research UK has got several articles debunking common cancer myths. One of the ones I have come across rather repeatedly is that acid environment causes cancer. So people should eat alkaline food. Like... Uhm... Lemons? Really? Lemons?! Yeah, lemons. That famous alkaline fruit. With pH of 2.0, wait... you mean that is not how it works? Somehow the proponents of alkaline diet to cure cancer suggest that lemon becomes alkalotic when you digest it. That somehow gastric acid (pH of 1.0 - 2.0) cancels out the citric acid. I am not sure what biology, or chemistry classes these quacks have been going to but they need to get a refund for that.
The body self-regulates its acid-alkaline level. The body maintains a very strict pH of 7.35 - 7.45. Go below that and you go into acidosis and go above that and you go into alkalosis. Both can and will kill you. A glass of lemon water is not going to do anything to shift it either way.
And honestly guys. The same goes for Bicarbonate of Soda. That excellent baking ingredient and cleaning material. The same doofuses who talk about cancer being acidic also advocate that people eat a whole load of Bicarb. You might neutralize you gastric acids for short period, and given the quantities, you would have to eat in order to do anything to cancer cells you would also neutralize your vital statistics.
I do have a lot of people on my FB friend list and a lot of them are well-meaning. But sometimes they share memes that are more harmful than helpful. I have seen a lot of people share memes and quackery articles that usually have something to do with 'XYZ kills cancer cells, scientismints prove!'. The problem with that is that ANYTHING will kill cancer cells in a petri dish, including washing up liquid. You are not going to cure cancer with washing up liquid. In vitro studies can be interesting, but sadly do not translate into the real complex systems like the human body. For example, a popular meme walks about cannabis killing cancer. Again at Cancer Research provides an excellent article laying out the truth regarding Cannabis, it uses in cancer treatment and what current evidence says about it. Cannabis has been found to be very useful in managing nausea, pain, anxiety and other side effects from the cancer treatment. But it is still not the cure for cancer.
Then there is this thing that cranks want to discuss called Vitamin B17. Can I just clear things up? There is no such thing as Vitamin B17. What these con people are referring to is a substance better known as amygdalin. Amygdalin is a perfectly natural compound which is found in apricot kernels, lima beans, clover, peach stones and many many more. When consumed amygdalin converts to cyanide. It is not a vitamin. It will kill you, I suppose in a way it does kill cancer.
What people sometimes have to bear in mind when they read miracle stories about cancer is the phrase Spontaneous Remission. Basically this is where cancer starts to improve for no discernible reason, it does happen. But it happens really, really seldom. Currently the statistics surrounding this is 1 in 100,000. If you know someone who this has happened to then be happy for them, but be vary of any talk about alternative therapies.
These vultures need to be stopped.
One of the main points to keep in mind regarding cancer is that there are at least 100 different types of cancers known. Each with their own pathophysiology's, each with their own characteristics and each with different ways of treatment. So when you see someone that claims that they can cure cancer or know how. Ask them which type of cancer, then ask them how.
 |
| Chronicle Flask |
The body self-regulates its acid-alkaline level. The body maintains a very strict pH of 7.35 - 7.45. Go below that and you go into acidosis and go above that and you go into alkalosis. Both can and will kill you. A glass of lemon water is not going to do anything to shift it either way.
And honestly guys. The same goes for Bicarbonate of Soda. That excellent baking ingredient and cleaning material. The same doofuses who talk about cancer being acidic also advocate that people eat a whole load of Bicarb. You might neutralize you gastric acids for short period, and given the quantities, you would have to eat in order to do anything to cancer cells you would also neutralize your vital statistics.
 |
| XKCD: Cells |
I do have a lot of people on my FB friend list and a lot of them are well-meaning. But sometimes they share memes that are more harmful than helpful. I have seen a lot of people share memes and quackery articles that usually have something to do with 'XYZ kills cancer cells, scientismints prove!'. The problem with that is that ANYTHING will kill cancer cells in a petri dish, including washing up liquid. You are not going to cure cancer with washing up liquid. In vitro studies can be interesting, but sadly do not translate into the real complex systems like the human body. For example, a popular meme walks about cannabis killing cancer. Again at Cancer Research provides an excellent article laying out the truth regarding Cannabis, it uses in cancer treatment and what current evidence says about it. Cannabis has been found to be very useful in managing nausea, pain, anxiety and other side effects from the cancer treatment. But it is still not the cure for cancer.
Then there is this thing that cranks want to discuss called Vitamin B17. Can I just clear things up? There is no such thing as Vitamin B17. What these con people are referring to is a substance better known as amygdalin. Amygdalin is a perfectly natural compound which is found in apricot kernels, lima beans, clover, peach stones and many many more. When consumed amygdalin converts to cyanide. It is not a vitamin. It will kill you, I suppose in a way it does kill cancer.
What people sometimes have to bear in mind when they read miracle stories about cancer is the phrase Spontaneous Remission. Basically this is where cancer starts to improve for no discernible reason, it does happen. But it happens really, really seldom. Currently the statistics surrounding this is 1 in 100,000. If you know someone who this has happened to then be happy for them, but be vary of any talk about alternative therapies.
Saturday 14 April 2018
Carpe, The Kings are dead, long live the kings.
Last night my other half and I attended what was in some ways a very sad night at Yorkshire Taps. The night was called Carpe Noctem, the last gig by the local kings of the music scene Carpe. These guys had been playing together for almost a decade and decided that enough was enough and have now called it a day after entertaining crowds with their funk laden grooves and joyous attitudes. First time I ever became aware of them was during the Lancaster Music Festival in 2014, and I have to say I was rather smitten from the get go. I wasn't the only one. These guys released one monster of an album during their career, they were the very definition of a band that should have got bigger.
From a purely musical perspective these guys were one of the most original composite bands I have had the pleasure of listening to. The mix of funk, jazz, hip hop, blues and hard rock with big band sentimentalities was all played with such confidence and relish. It could be argued that Flash is the front and centre of the band but that would be doing injustice to the rest of them because they all play such significant roles.
For example I remember seeing Carpe playing with Frenchie, the guitarist and singer, and they had to replace him with three other people. Jon Moore on lead guitar, is, well... Wow, those guitar solos were really rather awesome and never out of place. Frenchie's subtle rhythm guitar playing can't be underestimated, underpinning a lot of the songs. Has to be added that Flash is an excellent rapper, but they also have three really rather excellent singers who all have different styles but complement each other almost perfectly. Dave, Grum and Rachel's rhythm underpinning everything.
The thing that will stand out most is that what these guys wanted first and foremost was to have a good time and to make sure that everyone else did as well. I am going to miss knowing that they will be playing a gig locally.
From a purely musical perspective these guys were one of the most original composite bands I have had the pleasure of listening to. The mix of funk, jazz, hip hop, blues and hard rock with big band sentimentalities was all played with such confidence and relish. It could be argued that Flash is the front and centre of the band but that would be doing injustice to the rest of them because they all play such significant roles.
For example I remember seeing Carpe playing with Frenchie, the guitarist and singer, and they had to replace him with three other people. Jon Moore on lead guitar, is, well... Wow, those guitar solos were really rather awesome and never out of place. Frenchie's subtle rhythm guitar playing can't be underestimated, underpinning a lot of the songs. Has to be added that Flash is an excellent rapper, but they also have three really rather excellent singers who all have different styles but complement each other almost perfectly. Dave, Grum and Rachel's rhythm underpinning everything.
The thing that will stand out most is that what these guys wanted first and foremost was to have a good time and to make sure that everyone else did as well. I am going to miss knowing that they will be playing a gig locally.
Monday 9 April 2018
Metal Nurse Sojourn: Part 3, Sofia and getting lost in the woods
| Lost In The Woods |
The next day I got up early, got packed up, paid the hostel and set off to find that mysterious bus station again. In order to head back to Sofia. My other half had said that getting a bus was both quicker and cheaper, and of course provided better sightseeing opportunities than a train. Seeing as she had done a helluva lot more travelling than me, I took her word for it. She was correct. Getting the ticket was a bit of a trick, seeing as the lingua franca is Russian, but I did manage to obtain one. Then there was a bit of a misunderstanding regarding the seats, as I hadn't clocked on that that the seat numbers were on the tickets. Somehow I had expected it to be similar to the British system where people just plonk their butts anywhere. I got a mournful look from a Bulgarian grandmother and an international sign language explanation from another. The bus was full, and it was hot. And it only got hotter by the minute because the bus driver didn't want to open any windows or turn on the AC. It became very hard to keep my eyes open.
 |
| Hostel Mostel in Sofia |
After my kip, I go back to the common room of the hostel, get shown a map of where to go, where to eat and what there is to see. Then also with some aid from Google, off I trot.
 |
| Monument To The Soviet Army |
Oh and the monument, sadly scrubbed clean. Still nice and well done and fascinating to walk around and look at. Just not pop-culture referencing nice. So time to walk some more. Oooo, a squirrel... A BLACK SQUIRREL. That looks like a red one! Maybe we should import those into the UK. Oh, but it is the same species as the red one. Never mind then. Damn it was cute though.
The weather is still very nice so I just take my time to walk around the parks of Sofia. It is a nice city, good to spend a couple of days at. But to be honest, Plovdiv was nicer. Sofia is also slightly more expensive but that isn't really saying an awful lot. The one detail I did notice about Bulgaria is that there is not a lot of microbreweries. Which saddened me a little, there are some nice cheap lagers to be had. There was a lot of choice in vodkas and wines, but I prefer my ales. The city is alive, smells clean, and is not crowded with too many tourists. I know there are tourists around because the hostel is teeming with them. But it's not overrun with them like Prague. After much walking, I return back to my hostel to do some more writing and eat.
 |
| Sofia Day One |
 |
| National Museum of History |
I don't think I w
ant to press my luck too much. But I did manage to get into the museum. Which was captivating, the history of Bulgaria is an intriguing hotchpotch of different cultures amalgamating together. The Greeks have been here, The Romans, The Thracians, Bulgarians, the Ottomans and many more. Invaded by Hungarians, Mongolians, Serbs, and many more still. Then of course as can be seen above they have had a lot of input from the Soviets. Then there is the history of the Cyrillic alphabet itself, which remains the only alphabet where we can trace it back to its original creator, Clement of Ohrid. After taking another moment to stop and have some coffee, I take in the view. Specifically, the mountain that Sofia is based right next to. I want to take a photo up there. So again after consulting with Google Maps (Even though it probably did try and get me killed before), I vacate the museum after spending a good two hours walking around. On my way out the guard eyes me up suspiciously with a cigarette in his mouth, doughnut at hand and a big gut. Probably feeling like he should be doing his job, he asked me to hand my bag over so he could search it. Thankfully I only had bottles of water and some apples. Which I had purchased on the way. Which happens to be water from the Devin province, which considering my ultimate purpose of the trip just seemed to make sense. He seemed very disappointed by that.
I still hadn't made my way to Boyana Church so I start walking and sweating slightly. On my way there I come across a guy walking his pet cow. Boyana Church as mentioned previously was originally built in the 10th century, with various add-ons attached since then. It is on the Unesco Heritage List, it's a beautiful little church located again in a beautiful piece of the country. But again because of budget constraints I couldn't afford to enter but had a good mooch around the building itself. I do now wish I had paid to go in because the frescos in there are so unique and breath taking. After getting my breath back I then decide to walk up to "Жива вода Бояна" which according to Google Translate means "Living Water Boyana". Whilst there I promptly get a little lost in the woods. But I took my time in being lost, the surrounding nature and the woods were just too good to not to do so in.
 |
| The Snail House |
 |
| Church of Saint John Rila/ Lada / Abandoned Bus Shelter |
 |
| The Woods at the foot of Vitosha |
I sit down. Read a little bit and write a bit more. Get to bed and fall asleep. The next day I packed everything up and headed back home. Happy.
Friday 6 April 2018
Metal Nurse: Alcohol Free For The Year
On the 1st of March, I decided to take a sabbatical from alcohol. Not because I am an alcoholic, but because I don't want to become one. In the past year, I have found that my consumption of beer has gone up. I could see how easy it is to go from just having one, to JUST having two, to JUST having three. This would just start the occasional evening, slowly creeping up to every evening. Working where I work I have taken care of plenty (too many) people who are there because of alcohol. And every time I think "I don't want to end up like that". To end up having to take medications to assist you through the withdrawals, end up having seizures because said alcohol withdrawal. Running the risk of developing Hepatic Encephalopathy. Hooked up to a vitamin drip, plus other intravenous fluids because chances are that you will also be severely hydrated because the alcohol has depleted your vitamins and electrolytes from your body and brain. Taking copious amounts of laxatives in order to prevent the build-up of ammonia in your body.

Yes, I am not an alcoholic and I didn't feel like I am becoming one. But quite frankly I didn't want to risk becoming one. It just doesn't feel worth it. There isn't just the physical health side of things to consider there is also the mental health aspect of it. For many it is a form of coping mechanism to drink excessively, to suppress their depression and hide their anxiety. Without actually being aware that it is making both of those worse. Long-term excessive drinking can and does lead to psychosis and dementia. To go from wanting a drink to needing a drink, when you feel jittery and shaking, which doesn't stop until you've had your breakfast consisting of last nights unfinished booze. If you already suffer from depression/anxiety you run the risk of making it worse, and if you don't suffer from those debilitating illnesses you run the risk of developing them. Then there is the public health implication. In the UK excessive alcohol consumption costs society as a whole a whopping £21 billion. In the US the number is $249 billion, and that was in 2010, I can't imagine that that number has gone down since. WHO estimates that alcohol accounts for 5.1% of the total global disease burden, in 2012 over 3 million died due to alcohol-related conditions.

I know that there is also that rumour that it helps to relax, but I am not so sure anymore. I didn't actually find that it does. If anything I feel more stressed, especially the day after, my sleep is more disrupted and I am even grumpier when I wake up. All good research also shows that. You don't get enough sleep. You don't get enough REM sleep, it disrupts your circadian rhythm because alcohol relaxes your muscles it makes you more prone to sleep apnea, etc etc. Recent research have been implicating lack of sleep as one of the causes of ill mental health, as opposed to a symptom. So it all seems a little circular. I felt it was time to smash that circle. I like my sleep, and I prefer my sleep to be undisturbed. I especially didn't want to have to wake up several times just to have to empty my bladder. I want to wait at least another 50 years until that has to be a feature in my life.

Even just looking at the health evidence of all the ill effects that alcohol does to your body and mind. Alcohol has been linked to an increased risk of cancer development. At least 7 different ones, including breast cancer, bowel cancer and liver cancer. Drinking also increases your risk of developing cirrhosis of the liver, which itself is a risk factor in developing cancer of the liver. There is also increased the risk of developing acute pancreatitis, which itself leads to chronic pancreatitis, which in turn increases your risk of developing pancreatic cancer. Alcohol also adversely affects the cardiovascular system. It increases your risk of developing hypertension, coronary heart disease and peripheral vascular disease. All of which also increase your risk of stroke and heart attacks. You run the risk of developing Wernicke's Encephalopathy, which is caused by depletion of thiamine, this condition often precedes a condition called Korsakoff Syndrome. The more I read and the more I think about it, it just doesn't feel worth it.
Plus it's expensive. I don't particularly like the day after feeling, not just the full-blown hangover. But that 'bleurgh' feeling without a headache. Even without thinking about all the physical health issues, it just doesn't feel worth it. But giving up the alcohol. That does feel worth it.

Yes, I am not an alcoholic and I didn't feel like I am becoming one. But quite frankly I didn't want to risk becoming one. It just doesn't feel worth it. There isn't just the physical health side of things to consider there is also the mental health aspect of it. For many it is a form of coping mechanism to drink excessively, to suppress their depression and hide their anxiety. Without actually being aware that it is making both of those worse. Long-term excessive drinking can and does lead to psychosis and dementia. To go from wanting a drink to needing a drink, when you feel jittery and shaking, which doesn't stop until you've had your breakfast consisting of last nights unfinished booze. If you already suffer from depression/anxiety you run the risk of making it worse, and if you don't suffer from those debilitating illnesses you run the risk of developing them. Then there is the public health implication. In the UK excessive alcohol consumption costs society as a whole a whopping £21 billion. In the US the number is $249 billion, and that was in 2010, I can't imagine that that number has gone down since. WHO estimates that alcohol accounts for 5.1% of the total global disease burden, in 2012 over 3 million died due to alcohol-related conditions.
I know that there is also that rumour that it helps to relax, but I am not so sure anymore. I didn't actually find that it does. If anything I feel more stressed, especially the day after, my sleep is more disrupted and I am even grumpier when I wake up. All good research also shows that. You don't get enough sleep. You don't get enough REM sleep, it disrupts your circadian rhythm because alcohol relaxes your muscles it makes you more prone to sleep apnea, etc etc. Recent research have been implicating lack of sleep as one of the causes of ill mental health, as opposed to a symptom. So it all seems a little circular. I felt it was time to smash that circle. I like my sleep, and I prefer my sleep to be undisturbed. I especially didn't want to have to wake up several times just to have to empty my bladder. I want to wait at least another 50 years until that has to be a feature in my life.

Even just looking at the health evidence of all the ill effects that alcohol does to your body and mind. Alcohol has been linked to an increased risk of cancer development. At least 7 different ones, including breast cancer, bowel cancer and liver cancer. Drinking also increases your risk of developing cirrhosis of the liver, which itself is a risk factor in developing cancer of the liver. There is also increased the risk of developing acute pancreatitis, which itself leads to chronic pancreatitis, which in turn increases your risk of developing pancreatic cancer. Alcohol also adversely affects the cardiovascular system. It increases your risk of developing hypertension, coronary heart disease and peripheral vascular disease. All of which also increase your risk of stroke and heart attacks. You run the risk of developing Wernicke's Encephalopathy, which is caused by depletion of thiamine, this condition often precedes a condition called Korsakoff Syndrome. The more I read and the more I think about it, it just doesn't feel worth it.
Plus it's expensive. I don't particularly like the day after feeling, not just the full-blown hangover. But that 'bleurgh' feeling without a headache. Even without thinking about all the physical health issues, it just doesn't feel worth it. But giving up the alcohol. That does feel worth it.
Subscribe to:
Posts (Atom)









